I recently attended the third annual San Diego Pain Summit (I’ve been to all three!) and was fortunate to be the patient demo for Peter O’Sullivan‘s Cognitive Functional Therapy workshop. (for a review of the whole workshop, check out Diane Jacob’s post.)
Funny thing was, heading into it I thought I was going to be the wrong kind of patient because I know too much about pain science (ha! Like I know anything at all!).
But I have been having new pain in my left hip, pain that has been eerily similar to the pain I had in my right hip at the start of all this chronic pain business. It started in summer and was intermittent up until December where it became near-constant to constant. And I’d started having low back achiness across my whole low back starting in December.
But Peter didn’t start there, I just wanted to provide some context. He started with:
Tell me your story
It seems so simple yet it’s so profound. Tell me your story. THIS was the most powerful part of the entire interaction, in my opinion.
Through all of the doctors and therapists I saw over the years, not one had ever asked for my story. Sure, I’d been asked ‘tell me about your pain’ or ‘what brought you here today’ or ‘tell me about yourself’ – but as similar as they may seem they are WORLDS apart in my book.
We are the story we tell ourselves, after all.
Such an opening allows us to tell what is most salient for us at that moment in time. It might be what we value most, our beliefs about our pain, or what our worries are.
That simple question can tap into our identity and self-worth, our hopes and our fears. It taps into what’s most important to us right now.
Being able to tell our story not only lets the practitioner know who we are, it lets us know who we are. It lets us tell the story of our very selves
What was my story?
I went right back to being a firefighter, to the seemingly inconsequential tweak in my right hip stepping off the fire engine. To the uncertainty and confusion and worsening pain. To not being able to sit (with no good explanation) for over two years. To the dark years that followed, my withdrawal from the world and eventual medical retirement.
I was fiercely defensive of my strength and ability, out to prove myself (yet again) that I’m worthy, strong, capable…whether to Peter, to the audience or to myself I don’t know.
It was emotional. Any time I go back there it is. As far as I’ve come, I also lost a lot to pain. My career, my identity, some relationships, a couple years worth of living.
Motivational interviewing and reflective listening
Peter listened with such interest and attention to my every word, despite being in a large well-lit room in front of 60 some folks, that it surprised me. He didn’t interrupt me. He offered assurances and asked gentle, guided questions. I felt heard and validated, believed and cared for.
(To clue you in to how meaningful this is to me, just typing those words has me in tears yet again.)
He gently guided me with questions and reflected my story back to me and how he understood it. There were tears, but plenty of laughter, too. I felt known. All of me. My vulnerabilities and my strengths (of which I think vulnerability is one!).
 I imagine this takes plenty of time, experience and confidence to do as well as he does, he’s a master. But it is a learnable skill, I can’t recommend enough taking some courses in motivational interviewing.
I imagine this takes plenty of time, experience and confidence to do as well as he does, he’s a master. But it is a learnable skill, I can’t recommend enough taking some courses in motivational interviewing.
Fears, worries, anxiety
He was able to tie experience of pain in my left hip to my fears of going back down that dark path again. To my worries, largely unvoiced til then, about losing everything again. Everything I’ve once again worked so hard to build.
The nonprofit, my volunteer work, writing this blog and my book. Snowboarding, hiking, being outside. Socializing, traveling, engaging with the world. All at risk, it seemed. Fears of not being able to sit, another surgery, more ongoing pain.
He told me it was understandable to go back there, how reasonable it was for my fears and worries to become so elevated when this new pain started. The pain in my right hip led to some really difficult times and tumultuous years, after all. To darkness and sadness and feelings of worthlessness and purposelessness.
To just a whole lot of less.
He picked up on my perfectionism, too. The constant beating-myself-uppedness, the negative self-talk. Such as chastising myself for thinking there might (must!) be something structurally wrong in my left hip now, too. Another FAI diagnosis on the horizon, another labral tear to surgically repair.
He assured me it was natural to worry about such things.
Rules and checking
We touched upon my movement and postural habits, too.
My movement habits include perfectionism just as much as my thoughts (I would like to say something self-disparaging but I’m trying to practice self-kindness instead).
I have rules about posture and movement, self-imposed but initially planted in my fitness and firefighter days and reinforced by all too many clinicians and trainers.
Even with *all that I know* and all that I preach about movement variability and there being no such thing as ‘good’ or ‘perfect’ posture or movement, I still revert back to sitting, standing, moving – hell, apparently even lying on the ground – in low-back extension. Chest up, shoulders back, hips rolled forward.
sigh
Why? Who the hell knows, we humans are weird. I’m not alone, though, many of us weird humans with pain paradoxically put ourselves into the very positions that provoke our pain. It’s as though we’re checking to see if it’s still there.
Wait, does it still hurt? *check* Yup. Still there. How ’bout now? *check* Yup. Still there. How ’bout now…
During our chat I was sitting in a very tense/guarded/protective position. I’ve been aware of my guarding/tension for years, I just haven’t hit upon how not to be that way (until now!).
These extended postures and ways of moving of mine are as though I’m holding myself up out of my hips, literally trying to get away from the pain.
Hopes, dreams, values
Even though I was hard on myself, Peter was not at all hard on me (well, at least at this stage. He hammered me with squats and lunges, but that comes later). He made me feel normal, validated, understood.
And through our chat he also elicited my loves and values, the stuff that is of utmost important to me. Being outside, snowboarding, volunteering, getting the nonprofit going, writing.. My boys, my friends, my family. Being able to go out and socialize, travel, play.
From a recent walk in my happy place
Connecting the dots
Together we recognized the parallels to ‘before’ and how that would understandably increase my threat levels and pain.
We discussed how starting the nonprofit, though an awesome and exciting venture, is also one that includes a lot of new stressors, worries and tasks and that pain often comes about in periods of big change.
We noted that the political climate surely wasn’t helping, either, especially with my propensity for worry and anxiety (I’m a master catastrophizer, after all!). I have gone through bouts of extreme sadness and worry since November.
We talked about how all this was tied into my guarding and tension and thus affected my movement and postures.
Anxiety, worry, tension, pain loops
Worry is my default mode and my anxiety issues predated my pain issues, though it was definitely exacerbated by pain. It is mostly manageable, though, meditation my greatest gift for coping with it.
But when either one goes up, pain or anxiety, it becomes a race to the top to see which can get worst fastest and becomes a vicious cycle that feeds upon itself. And both lead to increased tension, guarding, protective behaviors. My movement becomes limited, rigid, which in turn feeds into the pain and anxiety.
pain –> anxiety –> tension –> more pain –> more anxiety –> more tension –> even more pain…you get the picture ;)
Creating new posture and movement habits
How to break the cycle? Replacing the old habits with new ones.
He guided me into new ways of sitting, relaxing, standing, moving, lying that were not as provocative (and were cognitively difficult for me!).
I had to slump into my chair, which was WAY more difficult than you’d think, and breathe into my belly. Belly breathing is pretty freakin’ hard when you’re holding yourself up out of your hips with tension and bracing all the time.
So I worked on relaxing, slumping, sinking into my hips, breathing. All which are against my usual grain.
I got out of my provocative extended positions (not bad positions! Just sensitive ones for me at the present) and into flexed positions. I sat in a flexed position, stood in a flexed position, squatted in a flexed position, lunged in a flexed position, single leg squatted in a flexed position, hopped in a flexed/relaxed position.
THIS WAS WAY HARD! More cognitively so than physically but it was physically demanding, too. He hammered my left leg (I’m still a good firefighter and will just do what I’m told!) until it was fatigued.
Disconfirming beliefs
Throughout all this Peter asked if I could do all these things if my hip was structurally compromised, especially as I could do so without pain. And I could do them without pain in the flexed positions. Ironically when I did them in my habitual ‘good form’/extended position it was painful.
He gently asked if I’d be able to snowboard if I was structurally compromised, helping me to overcome my worry/fear that there was something structurally wrong while also helping me not to chastise myself for thinking something might be structurally wrong.
I had to repeat to him that I had a healthy body, a mantra I have continued to use daily since.
I practice my new habits daily, including as I type this and find myself creeping back into extension and gently reminding myself to slump, move, change it up. When I have an urge to check I do ragdoll if I’m standing or just fold over if I’m in my chair.
Easy enough, but hard, too.
I practice breathing throughout the day, not just while I’m meditating, and think about being relaxed in all of my movement, not just while snowboarding (where it comes easier to me).
Habits are hard to change, but we can change them. It just takes flexible persistence and self-kindness (just, she says).
I’ve done my exercises, too, but it’s really the habits I’m focused on, both my thought and my movement habits. That’s where I think the greatest impact can be had.
Summarizing it all
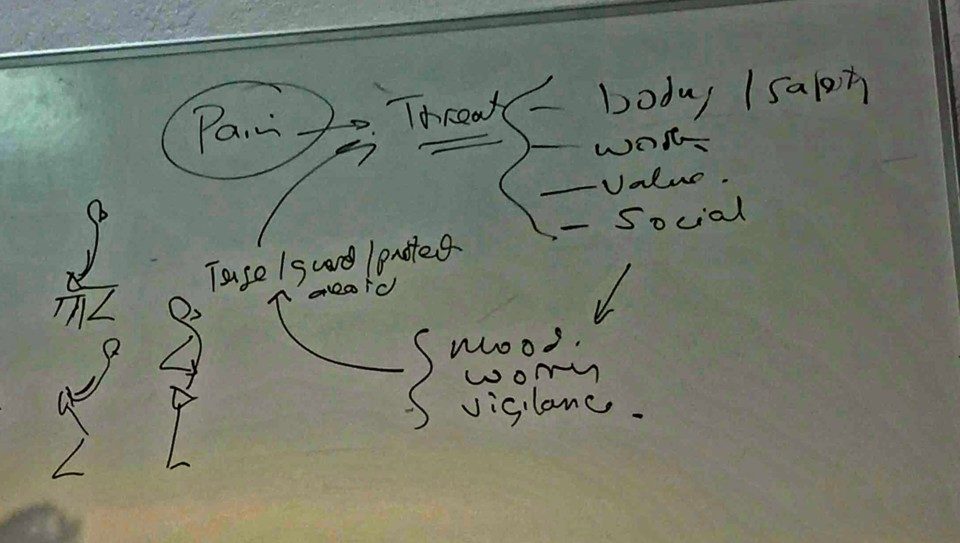
At the end of the session he wrote out my story on the whiteboard (shown above, the first was my story reflected back, the second my path forward). He connected the dots for me, as the gentleman in the patient demo the second day called it (and to which I fully agree).
He asked if he got it right. That, too, is IMMENSELY important. Because he might not have, but he did in my case. Even if he hadn’t, though, such a way of summarizing, reflecting and asking will let the individual say ‘heck no! Not at all!’ and help you get closer to what they meant.
I saw plainly, sketched out simply on that whiteboard, how much my left hip pain leads to fear, anxiety and worry, which leads to guarding and protection (none of this conscious, mind you), which leads to my extended habitual postures and ways of moving, which provokes my pain more (yep, it’s still there! There must be something wrong in there!), which leads to decreased movement variability and constant tension, which leads to more pain, which leads to more fear and anxiety and worry and so on.
And I saw plainly that I had a path forward, that there were things I could do to change my experience. With all that *I know*, I still have so much to learn. And it gives me so much hope, not just for me and my path but for all of us. Because I’m doing pretty damn well, I love my life, yet there’s still room for change and growth.
Imagine if I’d been through this earlier in my history? And imagine now where it will take me!
Sure sign of a successful session…
Gratitude
Peter’s compassion was palpable, as was his interest in my story, in me as a person, not just as a pain complaint or difficult pain presentation. It is such a contrast to some of my previous experiences.
Even though I was seen by many well-intentioned, good people, I often felt like I – me, Joletta, Jo – wasn’t a part of the equation. Just my pain, and subsequent expected improvement, mattered. Not me, not my life.
I was once referred to in a clinic as ‘the post-surgical hip’ in an overheard conversation, as though I was just a walking painful hip and nothing more, and of which I often felt I was. That sure didn’t feel like much.
So I am so incredibly grateful for this opportunity, grateful to Peter O’Sullivan for his time and care, and grateful to Rajam Roose and the San Diego Pain Summit for making it happen.
Going forward
My best strategy the last few years has been meditation for so many reasons (I use the Calm app now, which I adore and highly recommend).
Now I’m bringing what I’ve learned through meditation into my entire day. Relaxation, breathing, non-judgment, gratitude, acceptance of my current reality, being present, not catastrophizing about the future or living in the past, self-compassion.
I’ve known these things all along, but sometimes we need someone to connect the dots for us, to reassure us that we’re on the right path, to tell us that we’re strong, healthy, adaptable and capable.
That we’ve got this. And we do. We’ve got this.
For more of my experience after CFT with Peter O’Sullivan, read Posture and Movement Habits, Relax: Running after CFT, and the Power of Dialog and being able to tell our stories.




Pingback: Hyvää luettavaa ja katsottavaa / Biopsykososiaalinen lähestymistapa, CFT, vuorovaikutus – MoveDoc